There is a link between depression and brain inflammation
- and supplements can often help
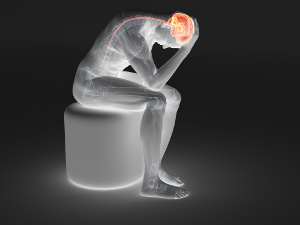 Depression is on the rise. The problem is often caused by inflammation in the brain. The British neuro-immunologist, Edvard Bullmore, has published the thought-provoking book called The Inflamed Mind, in which he describes the link between root canal treatment and depression, among other things. David Perlmutter, a neurologist, has written the book, Grain Brain, where he describes how gluten combined with carbohydrate overload also can cause inflammation in the brain. Depression, in other words, may occur when the blood-brain barrier is not as impermeable as assumed, and when the cytokines of the immune defense are able to cause undesirable brain inflammation. Numerous studies have shown that fish oil, vitamin D, magnesium, zinc, and selenium can improve a person’s mood by counteracting inflammation in the brain and other sites, and there is often a connection. It requires therapeutic doses, however, and it is vital that the supplements have good bioavailability, so the active substances reach the cells.
Depression is on the rise. The problem is often caused by inflammation in the brain. The British neuro-immunologist, Edvard Bullmore, has published the thought-provoking book called The Inflamed Mind, in which he describes the link between root canal treatment and depression, among other things. David Perlmutter, a neurologist, has written the book, Grain Brain, where he describes how gluten combined with carbohydrate overload also can cause inflammation in the brain. Depression, in other words, may occur when the blood-brain barrier is not as impermeable as assumed, and when the cytokines of the immune defense are able to cause undesirable brain inflammation. Numerous studies have shown that fish oil, vitamin D, magnesium, zinc, and selenium can improve a person’s mood by counteracting inflammation in the brain and other sites, and there is often a connection. It requires therapeutic doses, however, and it is vital that the supplements have good bioavailability, so the active substances reach the cells.
Edward Bullmore, who is a neuro-immunologist and a professor in psychiatry at the University of Cambridge, felt decidedly depressed right after undergoing a root canal treatment. This left him thinking about the underlying cause of his depression, which apparently was a result of inflammatory disturbances in his brain biochemistry. It is commonly known that bacteria can migrate to the bloodstream after a root canal treatment. If a person suffers from leaky gut, this can also happen. The immune defense is normally able to defeat these bacteria relatively quickly, but if it overreacts, it may cause chronic inflammation.
According to an article that mentions Edward Bullmore’s book, the blood-brain barrier is not as impenetrable as thought previously. Edward Bullmore claims that macrophages (white blood cells) in connection with different inflammatory conditions release cytokines, which are transferred to the brain by way of the bloodstream, and that may cause psychological problems such as depression. The problem is also described in a more recent article in the science journal Frontiers in Immunology.
In his book, Grain Brain, neurologist David Perlmutter addresses the fact that a poor digestive system and leaky gut may cause the body to absorb protein from gluten, milk and other foods that are not completely digested. In such cases, the immune defense may also react by launching inflammatory processes. Likewise, a carbohydrate-rich diet may cause insulin resistance, where the cellular glucose uptake is impaired. Insulin resistance causes the pancreas to produce more insulin, and the elevated insulin levels in the blood promote inflammation.
Overweight may also be a problem, as cells in adipose tissue are infiltrated with macrophages that release pro-inflammatory cytokines. There may also be other things that cause chronic inflammation such as autoimmune diseases, poisoning, and oxidative stress.
A review article in Nutrients from 2018 estimates that around 300 million people worldwide suffer from depression, and one billion people lack different nutrients, so it is relevant to take a closer look at the link between the two problems.
|
Fish oil is healthy
Omega-3 fatty acids are essential, as they are important for the nervous system, the cardiovascular system, and the immune defense. Fish oil contains the two omega-3 fatty acids called EPA and DHA, which are also present in our cell membranes, where they have a host of physiological functions.
Omega-3 fatty acids work in an intricate biochemical interplay together with the omega-6 fatty acids, and it is essential to get these two essential fatty acids in the proper balance. If we get too little omega-3, it sets the stage for inflammation. Harvard University researchers have conducted a study of 155 people with severe depression. The participants were given 1,060 mg of EPA, 900 mg of DHA, or placebo. After completing the study, the scientists could see that EPA had the greatest anti-inflammatory effect, which is why they offered the best effect against depression. Other studies show that fish oil lowers levels of CRP (C-reactive protein) and the two cytokines, TNF-alpha and IL-6, all of which are inflammation markers.
In the case of depression and other inflammatory conditions, it is a good idea to get 900-1,200 mg of EPA. Look at the label to see how many capsules to take.
It normally takes about a month before the optimal effect kicks in, which is why many people fail to see the connection and may give up too early. Always make sure to take fish oil that is within the approved safety limits in terms of peroxide value and content of environmental toxins.
|
Vitamin D, depression, and seasonal affective disorder (SAD)
Vitamin D is believed to control around 10 percent of our genes. Lack of vitamin D may therefore result in neurons, glial cells, and other cell types not being able to carry out their assigned tasks. Vitamin D also controls neurotransmitters such as serotonin and dopamine that are important for our mood. Vitamin D even inhibits several pro-inflammatory cytokines that are involved in depression. Scientists from Johns Hopkins University School of Medicine assume that vitamin D also prevents T lymphocytes from entering the brain. A large Irish study has shown that vitamin D-deficient people are far more likely to develop depression. The study also revealed that vitamin D deficiencies are very common, and that supplementation can improve mood significantly. Several other studies have also shown a link between depression and low vitamin D levels.
The reason why so many people at our latitudes are affected by depression is often their lack of vitamin D. During the winter period, the sun sits too low in the sky to enable vitamin D synthesis in our skin, and we only have limited amounts of the nutrient stored in our liver.
In Denmark, regular vitamin pills normally only contain about five micrograms of vitamin D, which is the daily reference intake (RI) level for adults up to 70 years of age. Many scientists claim that it takes a lot more to reach optimal blood levels of the nutrient (over 50 nmol/l). Our need for vitamin D may also be increased by factors such as old age, being dark-skinned, having diabetes, being overweight, or using cholesterol-lowering drugs (statins).
High-dosed vitamin D supplements with 20-80 micrograms are available on the market. Vitamin D is lipid-soluble so the best way to take it is in capsules where the nutrient is bound to oil. We also need magnesium in order to activate vitamin D in our liver and kidneys.
| It is a big problem that many people get too little sun during the summer period due to sun awareness campaigns. Health authorities fail to inform people about other ways of getting enough vitamin D. |
The link between blood levels of magnesium and the severity of depression
There is magnesium in kernels, almonds, nuts, whole grains, cabbage and other compact vegetables. Magnesium is vital for bone health and supports more than 300 different enzyme processes. An estimated 50-80 percent of the American population lacks magnesium, and we probably have similar figures in this part of the world.
In a study carried out by scientists at the University of Vermont, a clear link was observed between depression and having low serum levels of magnesium. According to the review article in Nutrients, various studies show that daily supplementation with 250-500 mg of magnesium may have a positive effect on mild to moderate depression. Several other studies show that magnesium may prevent and decrease depression by means of the following mechanisms:
- Increases the production of BDNF (Brain-Derived Neurotropic Factor), which is a growth factor for the hippocampus in the brain. Levels of BDNF are low in depression
- Functions as a gatekeeper in the cell membranes and blocks the NMDA (N-methyl-D-aspartate) channel that leads calcium into the nerve cells. Calcium flooding of neurons stresses the cells and disrupts their function in the synapses
- Counteracts oxidative stress
- Inhibits CRP and IL-6
- Helps regulate a malfunctioning gut flora and digestion that often follows in the wake of a depression
- Contributes to the body’s melatonin synthesis and improves sleep
- Helps the body produce serotonin, noradrenalin and dopamine
The essential balance between calcium and magnesium
Interactions between calcium and magnesium are fundamental to all living cells. As mentioned before, magnesium serves as a gatekeeper in the cell membranes, where it makes sure to allow the lion’s share of calcium to enter the cells in bones and teeth, whereas the cells in soft tissues like the brain, blood vessels, muscles and inner organs must be nearly devoid of calcium.
If the body lacks magnesium, the cellular calcium channels are left open with an overhanging risk of cells being flooded by calcium ions. This can stress the cells and cause them to go into a cramp and develop inflammatory conditions.
The jury is still out the question of determining the optimal balance between magnesium and calcium. In Denmark, the reference intake (RI) level for magnesium is 375 mg and 800 mg for calcium, which is close to a 1:2 ratio. In Japan, the ratio is closer to 1:1 because the Japanese consume more vegetables and no dairy products.
A magnesium deficiency is often a result of eating an unbalanced diet. Drinking large quantities of alcohol and using other stimulants, taking diuretics, and being stressed can also deplete the body’s magnesium levels. Insulin resistance and type 2 diabetes also leach the body’s magnesium. Many of the above-mentioned factors reinforce each other.
Many magnesium supplements, including Magnesia for constipation, contain inorganic magnesium oxide, which has poor bioavailability. It is far better to take organic magnesium compounds such as magnesium carbonate, magnesium acetate, magnesium orotate, magnesium citrate, or a combination of several organic magnesium sources. Most importantly, make sure the quality is okay, so the magnesium is properly absorbed in the small intestine.
| Too little magnesium and too much calcium (from dairy products and supplements) increases your risk of inflammation. |
Zinc and depression
Zinc is involved in around 1,000 different enzyme processes that are important for e.g. the brain’s chemistry and the immune defense. Zinc is also a powerful antioxidant that protects neurons against oxidative stress. Zinc is particularly important for the T helper cells of the immune system that control vast parts of the immune system.
According to the review article in Nutrients, the first links between zinc deficiency and depression were shown in the 1980s. Since then, several animal and human studies have confirmed the relation. A meta-analysis of 17 studies has found that zinc levels in the blood in patients with depression were lower than in healthy controls. Several other studies suggest that zinc deficiency affects the mood, especially in women.
Animal and human studies have also shown that zinc supplementation had a positive effect on depression and behavior in older people. Zinc supplements are even able to improve the effect of anti-depressive medication.
Zinc sources, widespread deficiencies, and supplements that work
Good sources of zinc are oysters, liver, meat, eggs, dairy products, nuts, seeds, kernels, and beans. Zinc from animal sources have the best bioavailability.
Zinc deficiencies are normally caused by unhealthy eating habits and lack of animal protein. High intake of iron, calcium, and alcohol also contributes to deficiencies. Ageing, celiac disease, diabetes, various types of medicine, and birth control pills can even increase the need for zinc.
In Denmark, the reference intake (RI) level for zinc is 10 mg, and the average diet only provides half that amount. Many zinc supplements contain inorganic sources such as zinc sulfate or zinc oxide, which the body cannot absorb very easily. Read the label and look for organic sources like zinc gluconate and zinc acetate that have good bioavailability. The European Food Safety Authority (EFSA) has set the daily upper safe intake level for zinc in adults at 25 mg.
| An estimated 25% of the world population is zinc-deficient. |
Selenium and psychological diseases
Selenium supports around 30 different selenium-containing proteins (selenoproteins) that are important for brain development, energy turnover, thyroid function, and the immune defense. Selenium also supports the important GPX antioxidants that protect against oxidative stress in the body. A review article published in StatPearls in 2019 shows that selenium deficiency may result in depression and aggressive behavior.
Science has also observed that certain neurotransmitters are affected by selenium deficiency.
A team of scientists from München has mapped out the mechanisms that are involved in the selenium-containing GPX antioxidants and their ability to protect brain cells (neurons) against death. Selenium deficiency is widespread in the Western world, mainly because of nutrient-depleted soil and exposure to mercury.
In Denmark, the reference intake (RI) level for selenium is 55 micrograms, but this may be too low.
Studies show that the daily intake of selenium should lie in the range of 100-200 micrograms. WHO has set the safe upper intake level for selenium at 400 micrograms per day.
You get the best bioavailability with organic selenium yeast that contains many different selenium species. This is similar to the natural variety you get from eating a balanced diet with different selenium sources.
| An estimated one billion people worldwide are selenium-deficient. |
Overweight, insulin resistance and type 2 diabetes
Overweight and diabetes are spreading like a bushfire, and a rapidly growing number of people are affected by metabolic syndrome, or pre-diabetes, which causes chronic inflammation, insulin resistance, elevated cholesterol levels, hypertension, and enlarged waist circumference. Depression is reported to be somewhat common among diabetics.
Since the 1970s, overweight individuals and diabetics have been advised to eat a low-fat diet with bread, potatoes, and other carbohydrate-rich foods. A recent Danish study, however, shows that it is far better for diabetics to eat a diet with fewer carbohydrates. This is supported by several international studies. Diabetics and people with sensitive blood sugar should try to eat les carbohydrate and more protein plus healthy fats, which the brain also needs. They should also make sure to get enough chromium that enhances the effect of insulin.
Chromium is found in foods like almonds, beans, nuts, fish, meat, and eggs. EFSA has stated that organic chromium yeast is up to 10 times more bioavailable than synthetic chromium sources like chromium picolinate and chromium chloride
Read the label before you buy chromium supplementsOrganic chromium yeast is absorbed up to 10 times better than chromium picolinate and chromium chloride. |
| Promotes inflammation | Inhibits inflammation |
| Too much omega-6 in the form of AA (arachidonic acid) | Omega-3 (in the form of EPA) |
| Oils from sunflower, corn, safflower, grapeseed plus margarine and industrially processed foods |
Oily fish and fish oil |
| Lack of micronutrients | Vitamin D, magnesium, zinc, and selenium |
| Too much carbohydrate and elevated insulin | Stable blood sugar and chromium |
| Overweight and enlarged waist circumference | Stable weight and a healthy weight circumference |
| Food intolerance | Healthy digestion and a diet devoid of foods that are not tolerated |
| Stress, physical inactivity, and too little sleep | Relaxation, moderate exercise, and plenty of sleep |
| IMPORTANT: Always consult your physician before discontinuing your use of anti-depressive medication |
References:
Rodkanal-blues fører til ny teori om depression. Tandlægebladet. 10.12.2019
Edward Bullmore. The Inflamed Mind. London Short Books 2018
David Perlmutter. Grain Brain. Yellow Kite. 2014
Chieh-Hsin Lee and Fabrizio Giuliani. The Role of Inflammation in Depression and Fatigue. Frontiers in Immunology. 2019
Jessica Wang et al. Zinc, magnesium, selenium and Depression: A review of the Evidence, Potential mechanisms and Implications. Nutrients 2018
Robert M. Carney et al: Baseline Blood Levels of Omega-3 and Depression Remission: A Secondary Analysis of Data From a Placebo-Controlled Trial of Omega-3 Supplements. Journal of Clinical Psychiatry. 2016
Rapaport MH et al. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: a proof-of-concept study. Molecular Psychiatry 2015
The Norwegian University of Science and Technology (NTNU). Understanding how omega-3 dampens inflammatory reactions. ScienceDaily 2017
Robert Briggs et al. Vitamin D Deficiency is Associated With an Increased Likelihood of Incident Depression in Community-Dwelling Older adults. J Am Med Dir Asso 2019
Alexander Muacevic and John R Adler: The Role of Vitamin D in Brain Health: A Mini Literature Review. Cureus 2018
Liam Davenport: Vitamin D Levels Predict Depression. Medscape Medical News 2015
Andrea Rosanoff et al. Essential Nutrient Interactions: Does Low or Suboptimal Magnesium Interact with Vitamin D and/or Calcium status. Advances in Nutrition 2016
Neil Bernard Boyle, Clare Lawton and Louise Dye. The Effects of Magnesium Supplementation on Subjective Anxiety and Stress – A systematic Review. Nutrients 2017
Role of magnesium supplementation in the treatment of depression: A randomized clinical trial. PLoS One 2017
Yves Rayssiguier et al. Magnesium deficiency and metabolic syndrome: stress and inflammation may reflect calcium activation. John Libbey Eurotext 2010
L-.E. Simental-Mendia et al. Effects of magnesium supplementation on plasma C-reactive protein concentrations: A systematic review and meta-analysis of randomized controlled trials. Current Pharmaceutical Design. 2017
Kido T et al. Inflammatory response under zinc deficiency is exacerbated by dysfunction of the T- helper type 2 lymphocyte-M2 macrophage pathway. Immunology 2019 Apr.
Ananda S Prasad. Zink in Human Health: Effect of Zink on Immune Cells. Molecular Medicine 2008
Aparna Shreenath. Selenium Deficiency. StatPearls. May 6, 2019
HERMHOLZ ZENTRUM MUNCHEN – GERMAN RESEARCH CENTER FOR ENVIROMENTAL HEALTH. Selenium protects a specific type of interneurons in the brain. EurekAlert 2017
https://diabetes.dk/diabetes-1/diabetes-og-psyken.aspx
Bispebjerg Hospital. Færre kulhydrater forbedrer type-2 diabetikeres evne til at regulere blodsukkeret. Nyhedsbrev 10. august 2019
Mads J Skytte et al. A Carbohydrate-reduced high-protein diet improves HbA1c and liver fat content in weight stable participants with type 2 diabetes: a randomized trial. Diabetologica. First online 23 July 2019
J. Racek et al: Influence of chromium-enriched yeast on blood glucose and insulin variables, blood lipids, and markers of oxidative stress in subjects with type 2 diabetes. Biological Trace Element Research. 2006
EFSA: Scientific Opinion on ChromoPrecise cellular bound chromium yeast added for nutritional purposes as a source of chromium in food supplements and the bioavailability of chromium from this source. EFSA Journal 2012
Pernille Lund. Sådan får du styr på dit blodsukker og din vægt. Ny Videnskab 2013
Search for more information...
- Created on .








